by Jasmine Khouja @jasmine_khouja
On the 17th November I attended the E-cigarette Summit 2016 at the Royal Society in London. The summit brought together researchers, policy-makers, smoking cessation services and industry members to hear about the latest research, developments and challenges in the e-cigarette domain.
The summit was a one-day event packed full of information with 20 fast-paced (10-20 minutes) talks and 4 panel discussions. My five take home points from the summit were:
- Communication
One point which was raised on multiple occasions was that good communication of the research into e-cigarettes is key to the public understanding the risks and benefits of e-cigarette use. Unfortunately, the consensus was that the communication of e-cigarette research to the public is poor. Astonishingly, one speaker commented that someone had asked their daughter: “Is your dad still selling e-cigarettes and killing people?” This demonstrates how badly e-cigarettes have been portrayed, despite general consensus that they are much less harmful than cigarettes. Researchers are trying to communicate their research but face hurdles; some journals may be less likely to publish articles that are positive about vaping, meaning that it is harder to publish evidence that vaping is not as bad for you as cigarettes. The media are also hampering researchers’ efforts as they prefer stories which are anti-vaping and sometimes draw inaccurate conclusions from the evidence, which makes for more interesting stories. However, effective communication of the research is possible: Professor Peter Hajek and Dr Alex Freeman provided some useful advice to researchers which included not inferring human risks from animal studies, ensuring risks are directly compared to those of smoking, being a trustworthy source by being competent, honest and reliable, and providing neutral information without recommendations allowing the public to make their own informed decisions.
- The British Medical Association’s Guidelines
Communication of the benefits and risks of e-cigarettes isn’t limited to publications and the media; doctors are being asked about e-cigarettes by patients. Despite the evidence that the research community has provided that e-cigarettes are less harmful than cigarettes, the British Medical Association are yet to update their guidelines to encourage smokers to switch to e-cigarettes. There seemed to be apprehension stemming from the lack of known long-term effects, despite the fact that we know there are vastly fewer and reduced amounts of toxicants in e-cigarettes compared to cigarettes meaning the likelihood of long-term effects as bad as or worse than smoking are extremely unlikely.
- Recent Research
Many new studies were presented but the study that really caught my attention was discussed by Dr Lynne Dawkins. Lynne provided evidence for increased puffing behavior when participants are given lower doses of nicotine in their e-cigarettes [1]. She concluded that inhaling more vapour to receive the same amount of nicotine exposes vapers to unnecessary amounts of toxicants. This is very topical as the regulations set out by the Tobacco Products Directive (TPD) which will be fully implemented by May 2017 limit doses to 20 mg/mL meaning that some higher dosage (36 mg/mL) users may expose themselves to extra toxicants to receive the levels of nicotine they need when the higher dosage product become unavailable in the next six months.
- The Tobacco Products Directive
The TPD provides some form of regulation for e-cigarette manufacturers and distributors. The inclusion of e-cigarettes in the TPD was controversial due to e-cigarettes not containing tobacco and the restrictive nature of the regulations which were seen as unnecessary by some users and industry members. Part of the regulations included the thorough testing of e-cigarette products to ensure they were safe and the publication of the contents (including toxicants) so that the public could make informed decisions. To my dismay, I was informed that the information submitted by the e-cigarette companies so far will not be made publically accessible for roughly six months due to a system error. I was also informed that compliance with the regulations was low and that age of sale restrictions in particular did not seem to be being enforced. The system and enforcement of the TPD in relation to e-cigarettes needs improving so that consumers can access the information which the TPD states they should have access to and to protect young people whose brain development may be adversely affected by consuming nicotine.
- New Systems
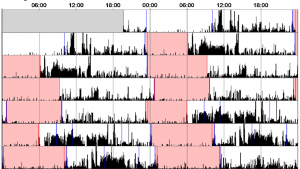
As restrictive as the TPD is, new products are still being developed. A new type of e-cigarette is emerging onto the market called pods. These devices are small and similar in size to older less effective designs of e-cigarettes (cigalikes) but have the power and nicotine delivery of the newer more effective tank systems. The sleek, compact designs combined with the improved nicotine delivery systems which prevent overheating (which is associated with harmful byproducts such as formaldehyde) are likely to be very popular. These systems can also record information on how the devices are used (how long individuals puff for and how many puffs they take etc.) which could provide essential information to researchers on how e-cigarettes are used in real life situations.
The day culminated in a key note speech by the Attorney General for Iowa, Tom Miller. He commended the UK’s focus on e-cigarette research and the general positive stance our public health officials have taken in terms of e-cigarettes. He concluded his speech by asking for help from the UK to bring the US up to the same standards.
References