Vicky Carlisle, who completed her PhD in TARG in 2021 has recently been interviewed about her research for the University of Bristol podcast. In the podcast, Vicky discusses her non-traditional route into academia as well as her research on the multi-level influences on recovery within opioid substitution treatment (OST). Vicky discusses the role of stigma and trauma as important barriers to recovery and retention in OST and her plans for developing an intervention to address stigma in OST
Involving the Public in Research: Taking the Mobile Lab on the Road
Amy Campbell, Hannah Sallis & Robyn Wootton
How do you feel about researchers tracking your mood using technology? How about tracking your physical activity or your sleep? How much technology will we let into our lives in the name of research?
These were the questions being asked this summer, when a team of researchers (from Bristol, Manchester, London and Oslo) went to speak to members of the public. They took the University of Bristol’s mobile lab around the city of Bristol and surrounding areas, to festivals, community groups and local parks. They wanted to understand public perceptions towards the use of technology to monitor mood and behaviour throughout the day, whether or not this was acceptable, and how to involve a diverse group of people in their research. In this blog post they tell us about what they did and what they found out.
What are your research interests?
We are an interdisciplinary group of psychologists, epidemiologists, statisticians and digital health researchers. We are interested in the links between health behaviours (such as smoking, alcohol consumption, exercise and sleep) and people’s mental health. To explore this, we usually use large cohort data, such as the Children of the 90s cohort (http://www.bristol.ac.uk/alspac/) or the MoBa cohort (https://www.fhi.no/en/studies/moba/). However, health behaviours and mental health are usually only assessed once per year at most, and reports are both retrospective and subjective. So, we have recently become interested in how we can collect better data. We all have smartphones in our pockets and many people wear smartwatches. We wondered whether we should be using wearable technology to collect more detailed real-time data on how health behaviours and mood change throughout the day.
What did you aim to find out from the mobile research lab?
Collecting real time data on mental health is a relatively new approach. As a result, new technologies are emerging and people’s attitudes are evolving. Therefore, before we started collecting data, we first of all wanted to speak with members of the public. We wanted to know if they would prefer using smartphones, smartwatches or smartrings for data collection. We wanted to know how frequently they would be happy to respond to questions and whether they would be happy to wear the devices all day.
We also wanted to speak with a more diverse range of people than usually take part in research. If we expect people to come into the University to speak with us, this will result in a biased sample – usually students or people who happen to live close to the University. Instead, we drove the mobile lab to different areas of Bristol, where people don’t usually take part in research. As a result, we reached a much more diverse group of people than we otherwise would. We hope that by incorporating diverse views into our research at this early stage, it will help us to engage more diverse samples when we come to data collection.
Where did you take the van and who did you speak with?
We headed out in the Bristol Mobile Laboratory with the aim of hearing as many different viewpoints as possible. The first stop was a bustling square in the centre of Bristol on a hot summer’s day. We were ready with a stall full of wearable tech, banners posing interesting questions about our research, and a fridge full of cold drinks. In such a busy location, it wasn’t long until we were chatting to many interested people.
These chats were informal, beginning by explaining our research aims and plans for the study. We were interested in people’s views on the project in general, but also their opinions on the specifics of the study. So, a conversation might begin by asking an open-ended question about people’s thoughts on tracking mood using wearable tech, before asking for feedback on specifics, such as how often people would be willing to answer questions about their mood, or whether there would be any barriers to people wearing the smart watches. Finally, we asked people whether they would be interested in providing their details to be contacted about taking part in this or other studies.
As we wanted to hear from as diverse a group of people as possible, it was important that we didn’t limit our conversations to those who lived in or visited central Bristol. With that in mind, we took the mobile lab on tour, visiting the local park in Keynsham, car boot sales in Hengrove and Marksbury, a coffee morning in Barton Hill, the pier in Weston-Super-Mare, and even made a guest appearance at Knowle West Fest (a local community festival).
These visits to different locations over the course of nine days meant that we spoke to a broad range of people with diverse ages, backgrounds, ethnicities, professions, and life experiences.
What did you find out?
There were many interesting perspectives from the public. We have organised these into those which related to the study design, the devices, and the questions.
- The study
The most important overall finding was that most people we spoke to were really keen to take part and thought our research question was interesting and important. It was really reassuring to know we were on the right track!
- The devices
Next, we were interested in finding out whether people would be happy to wear the devices (e.g., smartwatches, smartrings, other activity monitors). We used ballot boxes so members of the public could vote on their favourites – the rings were a clear winner, followed by the watches. We had some really interesting conversations about wearable technology, with the majority of people seeming keen on using these devices to measure their mood and behaviour.
There was a general feeling that it would be better not to show people their data during the study, people felt that being able to see fluctuations in their mood or their levels of sleep and exercise would influence their subsequent behaviour. Although most people we spoke to said they would like to see their data after the study. We are now working on the best way to return this information, so that it is interesting and useful for our study participants.
We were slightly concerned that we were planning to ask the mood questions too often during the day, and that this might get annoying. Our original plan was to ask 3 times during the day – morning, lunchtime, and evening. Most people we spoke to actually said they’d be happy to answer more frequently than that since it was just for a couple of weeks during the study. We had a couple of people suggest 5 times a day, or even hourly! It was really nice to find out that people were willing to devote so much of their time.
The main limitation that people mentioned around the devices, was that it could restrict people who work in specific roles from taking part in the study. For example, healthcare workers who cannot wear jewellery during their working day would be unable to wear the rings to measure their movement, or to interact with the watches to measure their mood. While these devices are likely to be a useful tool for research, and one that people are keen to use, we need to be mindful of certain groups that could be excluded from our studies as a result. Similarly, we also had several conversations about how we could ensure that older individuals are not excluded from these studies by making the devices easy to use and accessible. Currently we are planning to collect mood data by asking questions via smartwatches. One suggestion was to offer an alternative approach and allow people to hear the questions via pre-recorded phone messages. While this isn’t a viable option for our small feasibility study, this is important to bear in mind for future research.
- The questions
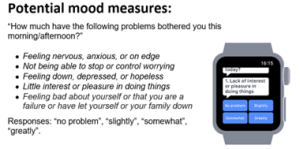
As well as asking people about the devices, we also wanted to get their opinions on the questions we should be asking. Originally, we had suggested using 5 questions to measure mood (these were taken from a 9-item depression questionnaire called the PHQ-9). We printed these questions out to discuss with people, and had some demo watches that ran through these questions.
(Image from Cormack F, McCue M, Taptiklis N, Skirrow C, Glazer E, Panagopoulos E, van Schaik TA, Fehnert B, King J, Barnett JH. Wearable Technology for High-Frequency Cognitive and Mood Assessment in Major Depressive Disorder: Longitudinal Observational Study. JMIR Ment Health 2019;6(11):e12814. doi: 10.2196/12814)
Most people felt the questions were easy to understand, although they didn’t like the first response option ‘no problem’. The question that people liked the least was the final question ‘Feeling bad about yourself or that you are a failure or have let yourself or your family down’. They felt that if your mood was already low, this question could be quite triggering, especially since all the mood questions were negatively worded. Based on this feedback, we have updated the mood questions, to remove this item and include some positively worded items. We have also updated the response options so that they are easier to interpret (not a lot, a little, a lot, extremely). Based upon feedback, we have also included a single item at the start of the questionnaire, which relates to overall mood: “How are you feeling overall right now?”. Individuals can respond to this item with a smiling face, neutral face or frowning face.
As well as questions on mood, we are interested in what is happening at the time people are responding. Originally, we had planned to ask about whether people had been exercising or sleeping, to check this corresponds with the information we get from the smart ring. Based on discussions while out and about in the van, we have updated this to also include information on significant events that had occurred, and social contact since loneliness came up in discussion multiple times.
One final point that came out of our discussion was that people were really keen to give us as much information as possible. For example, they wanted to be able to explain why they had rated their mood in particular ways – such as the reason for a poor night’s sleep or a significant event. We have now built a small qualitative component into the study, so we can incorporate this information into our findings.
Overall, how did you find the process of gathering public opinions and would you recommend it to other researchers?
We would absolutely recommend that other researchers engage in public involvement, especially trying to speak with as diverse a group as possible. The information we gathered has been extremely valuable in the design of our study, and has enabled us to identify an entirely new group of potential participants. The discussions highlighted several important points that we had not thought of, illustrating the importance of including different perspectives. We thoroughly enjoyed speaking to members of the public, it always reignites your passion for research! We are incredibly grateful to those who gave up their time – our study and results will be richer for this experience.
Affiliations
Amy Campbell is a PhD student in the Tobacco and Alcohol Research Group, at the University of Bristol. Hannah Sallis is a lecturer in the Centre for Academic Mental Health, Bristol Medical School and Robyn Wootton is a research fellow at Nic Waals Institute, Lovisenberg Hospital.
Acknowledgements
We are incredibly grateful to all of the members of the public who gave up their time to tell us their opinions. Their input is incredibly valuable to our future research. Thank you to the whole van team: Rebecca Pearson, Chris Stone, Alexandria Andrayas, Kimberly Beaumont, Ilaria Costantini, Miguel Cordero Vega, Tom Jewell and Nicky Wright, with additional thanks to Andy Skinner and David Kessler for their input on the research plans.
Funding
This work was supported by the Elizabeth Blackwell Institute, University of Bristol, the Wellcome Trust Institutional Strategic Support Fund, grant number 204813/Z/16/Z and a generous donation in memory of Jo Richardson. Robyn Wootton is funded by a postdoctoral fellowship from the South-Eastern Norway Regional Health Authority (2020024). Amy Campbell is supported by the Medical Research Council Integrative Epidemiology Unit (MC_UU_00011/7). This work was also supported by the European Research Council (Grant ref: 758813 MHINT).
Erasing the stain: Challenging the stigma of opioid substitution treatment. Findings from a stakeholder workshop

Author: Vicky Carlisle. Twitter: @Vic_Carlisle, Email: vicky.carlisle@bristol.ac.uk
On Wednesday 7th July 2021, I brought together key stakeholders with an interest in improving opioid substitution treatment (OST) from across the UK. This included people with lived experience, Public Health England staff, local authority public health practitioners, treatment service leads, pharmacists and academics. We discussed the findings of my recently completed PhD, and together we considered the next stages of developing an intervention to improve OST.
A summary of my research
For those not familiar with the topic, OST refers to the treatment of opioid dependency with either methadone or buprenorphine (alongside psychosocial support). Through my research, I wanted to understand what the key facilitators and barriers are to people ‘recovering’ in OST. To do this, I drew on both quantitative and qualitative methodologies. I found that loneliness, isolation and experiences of trauma and stigma were key barriers to recovery; whereas positive social support, discovering a sense of purpose and continuity of care were valuable facilitators.
Importantly, some factors appear to act as both facilitators and barriers to recovery in OST. For instance, I found that some service users used isolation as a form of self-protection (to shield themselves from negative influences), however this often left them feeling lonely and disconnected from the potential benefits offered by developing more positive social support networks.
Undoubtedly, the strongest barrier to recovery was stigma. Service users told me that they experience stigma from a range of sources, including from family and friends, healthcare professionals and members of the wider community. I found similar patterns in the literature review that I carried out (Carlisle et al, 2020). Stigma is like a stain where an individuals’ entire identity is defined by a single, negative attribute. In the case of OST, individuals may possess overlapping stigmatised identities of ‘OST service user’, ‘drug user’ and ‘injecting drug user’. Some will be further stigmatised due to experiencing homelessness, being HIV or Hepatitis C positive or through involvement in sex-work.
“I found that loneliness, isolation and experiences of trauma and stigma were key barriers to recovery”
Community pharmacies are one environment where service users report experiencing a great deal of stigma. Unlike customers collecting other prescriptions, many OST service users receive their medications (methadone/buprenorphine) through an arrangement known as ‘supervised consumption’. This means they must be observed taking their medication by a pharmacist to ensure that it is not diverted to others. This is often conducted in full view of other customers, despite guidelines which recommend that this takes place in a private room or screened area. This leaves OST service users open to the scrutiny of the ‘public gaze’.
My findings have several implications in relation to stigma. Firstly, OST service users receive poorer care than other members of society in healthcare settings, which may result in them avoiding seeking help from drug treatment and for other health conditions. Secondly, stigmatising OST service users makes community re-integration extremely challenging and this has been directly linked to individuals returning to drug using networks as it is somewhere they feel a sense of belonging. The ultimate impact of being repeatedly exposed to stigma is an internalisation of these judgements, resulting in feelings of shame and worthlessness – again impacting on individuals’ ability to seek help and develop supportive new relationships with others.
What we discussed during the workshop
Being able to present these findings to key stakeholders was a real highlight of my PhD work; it’s not often that you have the ear of so many invested and engaged individuals in one ‘room’ (albeit a Zoom room!). The findings of my PhD chimed closely with the experiences of those in the room and would be further reflected the next day when Dame Carol Black’s Review of Drugs Part 2 was published, which made specific reference to stigma.
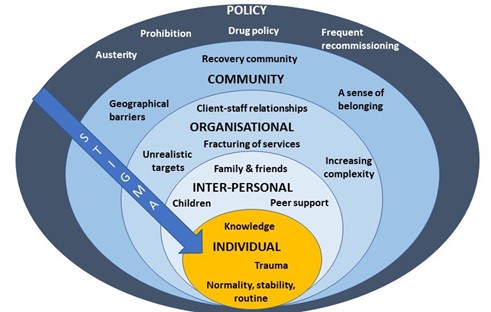
After I presented a short overview of my PhD findings, attendees spent time in small groups discussing how we might address OST stigma at each level of the socioecological system (see figure 1, above). A common thread that ran through each of the groups’ discussions was the importance of embedding interventions within trauma-informed frameworks. Attendees felt that increasing others’ understanding of the impact of trauma and ‘adverse childhood experiences’ (ACEs) may be a key mechanism by which to reduce stigma towards OST service users.
Indeed, a recent study found promising results in relation to this – that increasing the public’s awareness of the role of ACEs in substance use reduced stigmatising attitudes towards people who use drugs (Sumnall et al, 2021). Workshop attendees suggested that this outcome could be achieved through trauma-informed training of all individuals who might work with OST service users, such as pharmacists, the police and medical professionals, as well as those who work in healthcare settings, such as receptionists.
At the individual level there was a discussion about the way that stigma trickles down the socioecological system, resulting in self-stigma or internalised stigma. People felt that the best way to reduce this was to tackle stigma higher upstream first.
When thinking about reducing stigma in everyday inter-personal interactions, people highlighted the importance of using non-stigmatising language. For those who are interested (and I think we all should be!) the Scottish Drug Forum has published an excellent guide here.
Some excellent suggestions were made for reducing stigma that individuals experience in organisations such as pharmacies, hospitals and other settings. This is something that Dr Jenny Scott and I discussed in a recent article for the Pharmaceutical Journal (Scott & Carlisle, 2021). One attendee suggested the introduction of positive role-models within organisations who could be an exemplar of positive behaviour for others (a ‘stigma champion’ perhaps?). Training was identified as a key mechanism through which stigma could be reduced in organisations, including through exposure to people who use drugs (PWUD) and OST service users during training programmes. It was stressed however, that this should be carefully managed to ensure that a range of voices are presented and not just ones supporting dominant discourses around abstinence-based recovery.
Suggestions for improving community integration included increasing access to volunteering opportunities – something that people felt has been impacted by reduced funding to recovery services in recent years. It was also suggested that community and faith leaders could be a potential target for education around reducing stigma and understanding the impact of trauma, as these individuals may be best placed to have conversations about stigma with members of their communities.
Finally, there were some thoughtful discussions around the best way to influence policy to reduce stigma. The importance of showing policymakers the evidence-base from previous successful strategies was highlighted. Something that resulted in a lively debate was the issue of supervised consumption with arguments both for and against (this is also relevant at the organisational level). The group summarised that whilst diversion of medications was a risk for some, a blanket approach to supervised consumption and/or daily collections exposes individuals to stigma in the pharmacy, which leaves individuals vulnerable to dropping out of treatment. It was pointed out that supervised consumption policies were quickly relaxed at the start of Covid-19 restrictions – something that appears to have been done safely and with benefits to service users. It was also highlighted that supervised consumption in OST is inherently stigmatising, as users of other addictive drugs with overdose potential, such as other prescribed opioids and benzodiazepines, are not subjected to the same regulations. This sends a clear message to OST service users that they cannot be trusted. Other key suggestions were:
- Communicating with CQCs and Royal Colleges, who may be particularly interested in understanding how people are treated in their services.
- Drawing on existing stigma policies from other arenas e.g. mental health.
- Highlighting the fiscal benefits of reducing stigma to key decision makers.
- Tapping into plans for the new Police and Crime Commissioners, who have a trauma sub-group.
- Linking into work with ADDER areas, which may provide the evidence for ‘what works’.
What next?
I am now planning to apply for further funding to develop an intervention to reduce organisational stigma towards OST service users. The involvement of service users and other key stakeholders will be crucial in every step of that process, so I will be putting together a steering group as well as seeking out collaborations with academics internationally that have expertise and an interest in this area. I was really pleased to see that Dame Carol Black’s second report makes some concrete recommendations around reducing stigma towards people who use drugs. I hope therefore to be able to work with the current momentum to make OST safer and more attractive to those whose lives depend on it.
I’d like to extend my gratitude to all of the attendees at the workshop and to Bristol’s Drug and Alcohol Health Integration Team (HIT) for supporting this event. If you are an individual with lived experience of OST, an academic, or any other stakeholder working in this area and would like to be involved with future developments, please get in touch with me at vicky.carlisle@bristol.ac.uk or find me on Twitter at @Vic_Carlisle.
References
Carlisle, V., Maynard, O., Padmanathan, P., Hickman, M., Thomas, K. H., & Kesten, J. (2020, September 7). Factors influencing recovery in opioid substitution treatment: a systematic review and thematic synthesis. https://doi.org/10.31234/osf.io/f6c3p
Scott, J & Carlisle, V (2021). A pharmacy resolution for 2021: let’s improve the way patients with addiction are treated. The Pharmaceutical Journal. https://pharmaceutical-journal.com/article/opinion/a-pharmacy-resolution-for-2021-lets-improve-the-way-patients-with-addiction-are-treated
Sumnall, H. R., Hamilton, I., Atkinson, A. M., Montgomery, C., & Gage, S. H. (2021). Representation of adverse childhood experiences is associated with lower public stigma towards people who use drugs: an exploratory experimental study. Drugs: Education, Prevention and Policy, 28(3), 227-239. https://doi.org/10.1080/09687637.2020.1820450
Underestimation of Drug Use: A Perennial Problem with Implications for Policy

by Olivia Maynard
In a paper recently published in the journal Addiction, Hannah Charles and colleagues suggest that the prevalence of illicit drug use among 23-25 year olds in a Bristol-based birth cohort (ALSPAC) is over twice that reported in the Crime Survey for England and Wales (CSEW). The team propose that these figures reflect under-reporting in the CSEW, although they note that they may reflect higher levels of illicit drug use in Bristol. Here I present some preliminary data supporting their view that the CSEW underestimates illicit drug use.
In March 2020, I recruited 683 UK university students to participate in a short survey on drug use via the online survey platform Prolific which has been shown to produce reliable data. I recruited only students aged 18 to 24 years who reported using alcohol in the past 30 days, and participants reported whether they had used any of MDMA/ecstasy, cocaine or cannabis in the past two years.
Table 1. Prevalence of self-reported illicit drug use across three surveys of young people in the UK
| University students via Prolific Aged 18-24 |
Bristol, ALSPAC
Aged 23-25 |
CSEW
Aged 23-25 |
|||
| 2 years | 1 year | Lifetime | 1 year | Lifetime | |
| Any illicit drug usea | 52.7 (360) | 36.7 | 62.8 | 16.4 | 40.6 |
| Cannabis | 50.2 (343) | 29.2 | 60.5 | 13.8 | 37.3 |
| MDMA/ecstasy/amphetaminesb | 23.3 (159) | 17.0 | 32.9 | 3.6 | 11.1 |
| Cocaine | 21.1 (144) | 19.6 | 30.8 | 4.8 | 13.9 |
Notes: Values represent percentage of participants (number of participants). Percentages for CSEW and ALSPAC are taken from Charles et al (1) and are weighted percentages.
a ‘Any illicit drug use’ refers only to the illicit drugs assessed in the respective surveys (only cannabis, MDMA and cocaine in our survey), more drugs in ALSPAC and CSEW – see Charles et al (1).
b Our Prolific survey asked about ‘MDMA / ecstasy’ use, ALSPAC categorised ecstasy/MDMA use along with other ‘amphetamine’ use and CSEW asked about ‘ecstasy’ use.
Over half of my sample reported using at least one of cannabis, cocaine or MDMA in the past two years (Table 1). This is markedly higher than the CSEW’s estimates of either past year or lifetime use, and more in line with those reported in ALSPAC. Comparing across drugs, past two-year use of the three drugs is higher in my survey than either past year or lifetime use in the CSEW, and higher than past year, but lower than lifetime use in ALSPAC. Perhaps of more interest than ever use of the drugs over the past two years, I also examined the combinations of drugs students in my survey were using (Table 2). I find that the majority of students who report using illicit drugs have only used cannabis in the past two years (25% of all students), although the second largest group (15%) have used all three of cannabis, MDMA and cocaine.
Table 2. Prevalence of self-reported illicit drug among UK university students
| Qualtrics survey of university students (past two years) | ||||
| All (n=683) |
Female (n=336) |
Male (n=312) |
Other (n=35) |
|
| Illicit drug use | ||||
| Cannabis | 50.2 (343) | 48.5 (163) | 53.5 (167) | 37.1 (13) |
| MDMA / ecstasy | 23.3 (159) | 19.3 (65) | 29.2 (91) | 8.6 (3) |
| Cocaine | 21.1 (144) | 17.6 (59) | 26 (81) | 11.4 (4) |
| Illicit drug use profiles | ||||
| Alcohol only (no illicit drug use) | 47.3 (323) | 48.2 (162) | 44.6 (139) | 62.9 (22) |
| Any illicit drug usea | 52.7 (360) | 51.8 (174) | 55.4 (173) | 37.1 (13) |
| Cannabis only | 24.5 (167) | 27.4 (92) | 21.5 (67) | 22.9 (8) |
| Cannabis + Cocaine + MDMA | 15.4 (105) | 11.3 (38) | 20.8 (65) | 5.7 (2) |
| Cannabis + MDMA | 6.3 (43) | 6 (20) | 7.1 (22) | 2.9 (1) |
| Cannabis + Cocaine | 4.1 (28) | 3.9 (13) | 4.2 (13) | 5.7 (2) |
| Cocaine only | 0.9 (6) | 1.2 (4) | 0.6 (2) | 0 (0) |
| MDMA only | 0.9 (6) | 0.9 (3) | 1 (3) | 0 (0) |
| Cocaine + MDMA | 0.7 (5) | 1.2 (4) | 0.3 (1) | 0 (0) |
Notes: Values represent percentage of participants (number of participants).
‘Illicit drug use’ refers to participants reporting any use of the three drugs in the past two years.
‘Illicit drug use profiles’ refers to the combinations of drugs participants report using in the past two years.
a ‘Any illicit drug use’ refers only to use of cannabis, MDMA and cocaine.
There are some important differences between my sample and both the CSEW and ALSPAC samples. Some differences may mean that my figures are overestimates, including sampling university students who are more affluent than the general population (although drug use is not necessarily higher among students than non-students) and only including those who reported drinking alcohol (although according to the study authors, over 95% of the ALSPAC participants report past year drinking). Other differences may mean my figures are underestimates, including only asking about use of three drugs (thereby underestimating ‘any illicit drug use’), and the younger average age of my sample. I also report on past two-year use, rather than either lifetime or past year use as per CSEW and ALSPAC. Given these differences, I would like to run a larger, more representative sample on the Prolific platform (Prolific allows researchers to recruit a sample which is representative of the general population), to get an estimate of illicit drug use which is more comparable to ALSPAC and CSEW.
Despite these differences, my data support those reported by Charles and colleagues. Indeed, I find it unsurprising that illicit drug use is under-reported in the Home Office’s CSEW. The validity of self-reports for sensitive issues has long been a concern. Over-reporting of illicit drug use is not considered to be a concern and numerous methods have been developed for preventing under-reporting (see a 1997 NIDA report on this issue, as well as more recent techniques for estimating prevalence of use such as the crosswise method). It is important to consider the context in which surveys are administered, including participants’ perception of who is asking the questions and for what reason. It seems that if drug use is asked about in a research context, (e.g., with a clear research objective, informed consent and no possibility of repercussions), the validity of responses may be higher than when questions are asked by organisations that are perceived to be involved in the punishment of people who use drugs (e.g., governments, universities).
While the CSEW recognises that it does not reliably measure problematic drug use, my data and that of Charles and colleagues provide evidence that CSEW’s claim that it is a ‘good measure of recreational drug use’ may be wrong. Although it may be convenient to believe that only a small subset of the population uses illicit drugs, accurate information may galvanise policy makers (both nationally and locally, including at universities) into developing drugs policies that reflect reality and which support, rather than criminalise, the large proportion of the population who choose to use drugs. Indeed, this is what we’re doing at the University of Bristol, where it has been accepted that drug use is relatively common among our students and we’re providing support and education to those students who need it.
TARG’s top tips for wellbeing and productivity
Working from home can present huge challenges both to our work productivity and overall wellbeing. These challenges will vary in type and intensity from one person to another, and may also wax and wane at different times of the year.
Things we in TARG have been struggling with include:
- No separate workspace versus home space; blurring of boundaries between home and work
- Lack of motivation due to general stress or anxiety about the state of the world
- Material problems e.g. caring responsibilities, things in life disrupted by the pandemic
- The social aspect of not seeing people
- Difficulties in communicating and getting things done when we can’t be together in person
Although it is important to note that “it’s ok not to be ok”, there are things we can do that may help us feel better and/or be more productive in our work during these times.
With this in mind, and wanting to support each other as best we can, our group got together to share tips for coping with working from home.
Here is the TARG list of top tips for wellbeing and productivity:
Working Environment
- Set a designated working area and go to a separate space for breaks.
- Or, rotate your working area around different spaces for a change of scene.
- Keep your working environment tidy.
- It helps if you keep your home tidy too – it doesn’t have to be spotless though! Just things like making the bed and opening the curtains each morning helps.
- Have one day every week or fortnight when you tidy up your files and emails.
- If it helps you concentrate, listen to music or nature sounds or have the radio on. You could turn it off when you’re on a break, then restart it when you want to continue working. Spotify has lots of focus music playlists, or try YouTube.
- Try using earplugs or noise-cancelling headphones if you want a quieter environment.
- If you have to work from a laptop, try attaching a computer monitor and separate keyboard and mouse. The extra monitor extends your screen space making working easier, and also gives the feeling of using a separate ‘work computer’ helping to differentiate your personal laptop use from work time.
- Download a second web browser and use it only for work tasks. Keep only work bookmarks on your work web browser.
Emails
- Only check your emails two to three times a day at specific times.
- Add a message to your email signature such as “I check my email at 10am and 3pm every day so you will only hear from me at these times”. We don’t have to be constantly available.
- Don’t leave your email inbox open. Turn off notification sounds and popups.
- Work for an hour in the morning before checking emails.
- Glance at an email to see if it’s important but then ignore it until later.
- Flag emails and then answer them all in a block of time later.
Phone
- Only check your phone two to three times a day at specific times.
- Leave your phone out of sight e.g. in a drawer that’s out of reach.
- Turn off notification sounds.
- Remove work email apps from your phone.
Daily Routine
- Tailor your work schedule to your personal preferences – there’s no need to stick to 9 to 5.
- Whatever your preferred working schedule is, do have one, and stick to it.
- Schedule tea breaks at certain times of the day.
- Get ready and dress in the morning as if you were going to work.
- Go for a quick walk before you start work to simulate a commute.
- Have a proper lunch break, away from your working area if you can.
Task Scheduling
- ‘Eat the frog’: do the most difficult task of the day first.
- Block out a particular day for particular tasks.
- Schedule tasks that require more concentration to quieter times of the day.
- Set your tasks for the day each morning. Make them specific goals. Prioritise the tasks you need to do; don’t try to do everything.
- Or, schedule tasks per week rather than per day. Whatever works for you.
- If you’re struggling to start try to do just one task. Often once you start it’s easier to continue.
- Break up big tasks into smaller chunks and schedule them through the week.
- Make your day task-based rather than hours-based. E.g., “I will complete three tasks today” rather than “I will work seven hours today.” If you finish early, have the rest of the day off!
To Do and Done Lists
- Keep a ‘Done’ list to remind yourself of what you’ve achieved each day.
- If you start a task but haven’t finished it, have a symbol you can mark next to it so you can still see your progress.
- Have a symbol/colour to mark tasks that you’re waiting to hear back from others on before you can proceed.
- Colour code your to do list depending on task urgency.
- Break down tasks into micro-steps.
- Make your to do list visually appealing.
- Use Trello to make a to do list.
Motivation/Rewards
- Schedule time for activities you enjoy.
- Write a list of things you enjoy and use it as motivation.
- Gamify work: time spent working unlocks points that you can spend on fun/relaxing activities or treats. You could make a motivation board with stickers to record your points.
Meetings
- During meetings which are mostly just listening, do household chores that don’t take mental capacity (so you can still concentrate on listening) to have extra free time later.
- Attend a meeting from outside by using your phone. Sit in the garden, or go for a walk.
Maintain Clarity and Perspective
- Avoid foods at lunchtime that spike your blood sugar leading to lethargy in the afternoon.
- If things pop into your head (e.g. things to do, worries) note them down and set them aside for later.
- If you’re struggling to focus, take a break. E.g. go for a walk, have a nap or relax with a book. Set a timer for going back to work.
- Take a break every 10 minutes or use the Pomodoro Technique.
- Set a time limit for tasks and then move on (unless it’s urgent that you finish it).
- If you’re struggling to get anything done, sometimes it’s much better to just do the minimum amount and then stop, or allow yourself the day off and try again tomorrow. That’s ok!
- If you have a non-productive day, don’t be hard on yourself. Try speaking to yourself as you would a dear friend.
- We are all trying to just be as reasonably productive and motivated as we can in these circumstances – don’t expect as much from yourself as you would in normal times, and know that you are most definitely not alone in struggling.
Take Care of your Wellbeing
- Looking after your wellbeing is important in and of itself but also benefits productivity.
- There are lots of things we can do to improve our wellbeing, but we don’t want to turn those things into yet more ‘tasks to get done’. Rather than setting wellbeing goals, you could try simply recording what you do each day for your wellbeing, without judgment or expectation. By just recording these things, you may find you automatically start doing them more.
- Move: go for a walk, do some stretches, get up to make a cup of tea, walk around the garden.
- Sleep: try to get plenty of sleep, instead of working late ask yourself “can this task be finished tomorrow?”
- Rest: set aside a bit of time each day to rest and relax with whatever feels restful to you.
- Play: find time to do things you enjoy, having fun is important for adults as well as children!
- Gratitude: take a moment to think about something you are grateful for in your life.
- Nature: notice the nature all around us, even in urban environments there is plenty to see and hear.
- Pets: cuddling a pet releases endorphins!
- Laugh: listen to a funny podcast or watch a comedy show.
- Connect: share how you really feel with a trusted person. Resist the urge to pretend everything’s ok if it’s not. (But if you don’t feel like sharing, that’s ok too.)
Group Strategies
- Daily morning check-ins that anyone can pop in to.
- Socials (socially distanced outside when permitted by rules, otherwise online).
- Online coffee breaks and lunch breaks on Slack/Zoom.
- Continuing the schedule of regular meetings that we had before the pandemic, but online.
- Sharing our successes AND failures, it’s especially good if we can laugh about it!
- Using Slack for quick messages and to stay in touch socially with a dedicated social channel.
- One-to-one catch ups.
- Sharing goals for the day with each other and checking in at the end of the day/an hour later.
- Online writing retreats.
Incorporating new things into your daily routine can feel odd or an uphill struggle at first, but we humans are very good at building habits, so stick with it for a few days and it might become second nature. You could try picking one or two things from the list that resonate with you, and see how you go.
Thanks to the whole group for their contributions and especially to Jackie Thompson for holding the group meeting and co-ordinating responses.
We will be posting these tips on Twitter; if you’d like to see these regular reminders in your Twitter feed follow @BristolTARG or head to the #TARGWellbeing hashtag.
Take care everyone!
Reflections on a crisis – opportunities for a teaching overhaul
Written by Angela Attwood and Olivia Maynard, with reflections from Marcus Munafò
Beyond the immediate impact on people’s lives and livelihoods, the SARS-CoV-2 pandemic has caused a great deal of disruption in how we work. The burden on academics, particularly with respect to teaching, has been considerable. But are there positives that we can take from this situation?
Academia can be surprisingly conservative – we have ways of working that we are reluctant to change. While undergraduate courses may have been tweaked in response to student feedback, they remain largely unchanged from the courses available in the 1990s. Yet over this same period the ways that young people digest knowledge has changed radically. Today’s undergraduates are digital natives, used to receiving content in very different (and more flexible) ways.
Once we knew the pandemic would force us to move to online teaching, and that we’d be delivering our third-year optional psychology unit on ‘Drug Use and Addiction’ online, we knew we had to take the opportunity to completely overhaul our course and update our pedagogy.
We started by identifying key principles that would inform the redesign of the course. As we outline below, we aimed to: ensure clarity, maximise engagement, facilitate presence, tackle the “valuable but missable” problem of live sessions, and be flexible.
Our redesigned course followed a flipped lecture format, whereby asynchronous material was delivered ahead of an online live (synchronous) session. This flipped approach is known to have pedagogical benefits over traditional didactic lectures. This was a substantial structural change to our course, but throughout we tried to avoid reinventing the wheel! Rather we wanted to create a course that was pedagogically sound, based on current evidence, and shaped by our key principles.
The feedback so far from students has been overwhelmingly positive (perhaps even more so than in previous years!) and we strongly believe our principles have been key to the success of the course. We therefore want to expand on each principle and share what we have learned so far, in case this is helpful for others also faced with the daunting task of complete course redesign.
Principle 1: Ensuring clarity
More than anything else, it was essential that students understood what they needed to do and why they need to do it.
What we did:
- Created a consistent structure. We had folders for each sub-unit (previously lectures, but “sub-unit” better captures the granular nature of the content). Released weekly, these contained all teaching material (e.g., pre-recorded mini “lectures”, reading, etc.) for that week.
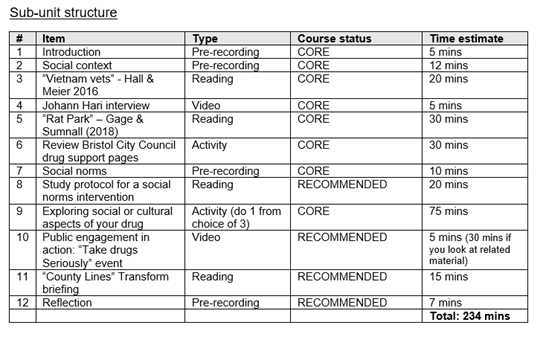
- Ensured requirements were clear. Each sub-unit started with a “roadmap”, including a summary of the sub-unit, intended learning outcomes, and an ordered list of tasks for completion, with an estimate of the time required for each.
- Clarified the importance of each task. We labelled these as either as CORE or RECOMMENDED. This allowed students flexibility, as they could choose to leave or return to RECOMMENDED items.
- Provided guidance notes for all academic reading (i.e., journal articles, book chapters). This included an overview (why it was chosen), any focussed reading (particularly useful for long review articles), and key “take home” messages *.
* This was an unexpected “win” as our discussion board inbox was significantly quieter this year. Many questions in previous years asked how to make notes on or read journal articles in the context of the course. The number of these questions received at the point of writing is zero!
Example sub-unit structure from one of the “roadmaps”
Student feedback
“The structure for the sub-units is SO helpful, really like how it tells you how much time each activity is going to take.”
“The pre-recordings are a very good length, and the little summary of everything we are doing for the sub-unit with the timings is incredibly helpful.”
Principle 2: Maximising engagement
Students are spending more time working at home, due to local or national restrictions, or limits on campus study space. This means that as well as material needing to be high quality, it also needs to be interesting and engaging. We focussed on material that was digestible, offered various methods of delivery, and gave students flexibility in how they structured their own learning.
What we did:
- Lectures recorded into bitesize chunks (ideally of no more than 20 minutes each). This reduced the burden associated with listening to each lecture and provided students with more flexibility when it came to organising their learning.
- Academic reading was supplemented with additional materials (e.g., videos, podcasts, websites). This allowed students to explore areas of personal interest more deeply if they wished to.
- Student-led activities (e.g., interview their friends, own literature searches, evaluate websites, mini-experiments). This provided opportunities for students to again explore areas of personal interest more deeply, in a range of different ways.
- Student choice (e.g., choosing a drug they were interested in, and activities that could be aligned to build a “portfolio” of materials specific to their drug of choice). This fed through to assessment where they could answer the question on any drug they wanted.
Student feedback
“I really like the sub-unit structure. As someone who doesn’t learn best unless there is a range of different learning stimuli in combination (e.g., lecture content, reading, visual cues like videos/stats graphs etc.) I find the subunits are so interesting and they help me to focus my energy onto the task at hand and stops me getting distracted.”
“I really enjoyed the variety and the fact it wasn’t just hours and hours of straight lectures which can get really dull! :)”
Principle 3: Facilitating presence
Working through material posted on a website can be isolating. It’s important to create a sense of community in online settings.
What we did:
- Used software that enabled student interaction and reflection throughout the week (e.g., Padlet, Mentimeter). We made sure at least one of these was present in each sub-unit, and encouraged students to communicate with each other as well as ourselves.
- Recorded “reflection” lectures between ourselves (lecturers) or invited guests. This ensured that students saw our faces during the week, as well as a range of different contributions from the wider academic community.
- Held weekly live sessions on Zoom to reflect on the week’s teaching. Although not strictly necessary, we both attended all live sessions to maximise our interaction with the students, and encouraged students to have their webcams on during these sessions (about half did).
- Held weekly live drop-in sessions (in addition to core live sessions) to answer questions and chat. This provided further opportunities to interact directly with ourselves and other students in real time.
- Used Zoom functions in live sessions – including breakout rooms – to give students a chance to talk to each other. We also used Zoom polling to ensure that all students had an opportunity to contribute, even if they didn’t feel like talking.
- Emailed the cohort regularly with additional opportunities, talks etc. relevant to the course. This created a sense of the wider academic community that they are part of, and the ongoing research activity relevant to the course.
Student feedback
“I really enjoyed the smaller rooms when on Zoom to talk to others in small groups of 5. Found it a lot easier to talk in these smaller groups than larger ones. I also liked the multiple-choice questions that you can present on the screen to see how everyone else is doing in terms of the sub units and the current work.”
Principle 4: Tackling the “valuable but missable” problem for live sessions
One of the biggest risks to any live session are technical issues. This created a “valuable but missable” paradox – we didn’t want to deliver core material during live sessions (so they could be missable if a student had Internet issues), but the sessions also had to be seen as valuable (or students might not attend!)
What we did:
- Constructed live sessions to be “skill building” (e.g., essay planning, argument building, debating skills, evidence synthesis and critique). These were designed to be valuable across the course as a whole, but any one could be missed with limited impact on assessment.
- Created different formats for the live sessions to make sure these were seen as valuable, but also interesting and engaging (e.g., discussion on how to answer a mock essay question, multiple choice quiz, hot topic debates).
Student feedback
“I really liked the quiz session last time, it made me think about the information I absorbed in the subunits, but equally I loved the debate. Practice essay questions are also very useful because I am struggling with planning my essays in general.”
“I think the live sessions have been very beneficial in a number of ways related to our essays, overall course understanding and guiding areas for reading.”
Principle 5: Being flexible (we are learning too!)
Co-design with end-users is vital for the best end-product. We allowed time to ask for student feedback, and space to respond to it.
What we did:
- Created polls that allowed students to vote on upcoming content (e.g., what question would be discussed in live sessions; what format of live sessions they find most helpful).
- Kept aspects of the course only partially developed (e.g., live session format) so that we had scope to be responsive to feedback.
- Continually asked for student feedback, via short polls and surveys on specific questions (e.g. ‘What should the format of the live sessions be?’, ‘How long should we stay in breakout groups for’) as well as asking for stop-start-continue feedback on the course as a whole, via an online survey that students could complete at any point during the course.
So, what does the future hold?
While we all hope ‘normal’ life will resume soon, the reality is that the world will not be quite the same post-pandemic. Much like many businesses that are planning to retain positive elements of home working, we should be open to retaining elements of our new ways of teaching. The crisis of the pandemic has created an opportunity to fundamentally overhaul and modernise the way that we teach that would have been unthinkable in a ‘normal’ year. And it seems to have worked – to quote a student, “It’s better than face to face teaching” (emphasis added).
We agree that these new ways of teaching are better – not just for students but for academics too. The recorded asynchronous material will stay current for 2 or 3 years (and perhaps longer for more introductory courses), meaning that if we retain this overall structure, our workload will be less next year. At the same time, many of the various synchronous elements can return to a face-to-face format, ensuring we spend more time in small groups, doing interactive work which both students and academics (certainly ourselves) find more engaging and fulfilling.
While our model is certainly not perfect – it had to be developed rapidly under considerable pressure – it’s a start, and offers a glimpse of the future.
Maximum cigarette pack size: a neglected aspect of tobacco control
Written by Anna Blackwell, Senior Research Associate
The manufacturing or importing of packs of cigarettes with fewer than 20 cigarettes per pack was prohibited in the UK when the EU Tobacco Products Directive and standardised packaging legislation were fully implemented in May 2017. This change was aimed at reducing the affordability of cigarettes and thereby discouraging young people from smoking. This directive also required the removal of branding and established a standard shape and dark green colour for packaging, including pictorial health warnings, which prevented the use of packaging for promotion and reduced its appeal.
However, the tobacco industry has been able to exploit loopholes in recent packaging regulations, including the absence of a regulated maximum pack size, by introducing non-standard and larger pack sizes to the market to distinguish products. This is a public health concern given evidence that larger pack sizes are linked to increased smoking, and could undermine existing tobacco control success.
In a recent Addiction Opinion and Debate paper, we proposed that a cap on cigarette pack size should be introduced; a pragmatic solution would be to permit only a single pack size of 20, which is now the minimum in many countries. This approach would reduce the number of cigarettes in packs in several countries such as Australia – where packs up to sizes of 50 are available – and prevent larger sizes being introduced elsewhere.
Capping cigarette pack size therefore has the potential to both reduce smoking and prevent increased smoking. While the health benefits of reducing smoking alone are small, it may have important indirect effects on health through its role in facilitating quitting. Those smoking fewer cigarettes per day are more likely to attempt to quit and succeed in doing so. Trials of smoking-reduction interventions have also found that these can lead to increased quitting when combined with nicotine replacement therapy.
Our Opinion and Debate paper drew on evidence from a range of sources including industry documents and analyses, population surveys, intervention trials and Mendelian randomization analyses. Together these suggest that consumption increases with larger pack size, and cessation increases with reduced consumption. However, direct experimental evidence is not currently available to determine whether pack size influences the amount of tobacco consumed, or whether the association is due to other factors.
People who want to quit may be using smaller packs as a method of self-control, and smokers who successfully cut down and later quit may be more motivated to do so. Cost is also an important factor and larger packs may be linked to increased smoking because they have a lower cost per cigarette. Further research is needed to determine whether the associations between pack size, smoking and cessation are causal to estimate the impact of policies to cap cigarette pack size.
Commentaries on our Opinion and Debate paper, published in the May 2020 Issue of Addiction highlight the need to understand the mechanisms for the associations observed between pack size and smoking in order to identify the optimal cigarette pack size. Although mandating packs of 20 is a pragmatic approach, pack size regulation needs to achieve a compromise between tobacco affordability and smokers’ self-regulation. Nevertheless, the policy debate should start now to address this neglected aspect of tobacco control.
To find out more visit the Behaviour Change by Design website or follow us on Twitter @BehavChangeDsgn @BristolTARG
Leaving the Lab: Rising to the Challenge of Remote Research
Written by Angela Attwood and Maddy Dyer
COVID-19 impact on research
The coronavirus (COVID-19) pandemic has forced millions of us to embrace remote working, and researchers are no exception. Universities are closed and face-to-face research with human participants has been temporarily halted. This has created challenges for our research, and laboratory and field studies are particularly affected.
As part of a large research group at the University of Bristol, we had to respond to this new situation and develop contingency plans for our research. Our first step was to review ongoing research and identify which studies could be suspended. We were fortunate on two counts: 1) we were able to put data collection on hold for many of our studies because there was enough flexibility in our planned completion times, and 2) we were able to stay busy with other work (such as analysing or writing up data from completed studies or developing new grant applications).
In all honesty, we would probably have stopped there with our contingency plans if it hadn’t been for one study that did not have this flexibility. This study investigates smokers’ experiences of switching to e-cigarettes, and requires participants to vape and complete various tasks across a two-week period. If we weren’t able to deliver on this study by a fixed deadline of the end of 2020, the funding would be withdrawn and one of our research staff would have been out of work. This forced us to think again…
Challenges and opportunities
There have been more challenges than opportunities in the context of the COVID-19 outbreak. However, one thing this global crisis has encouraged is innovation and creativity. We responded to the pressing need to complete this project by adapting our protocol so that the study could be run remotely (with no face-to-face communication). Some studies can move onto online platforms (and some of our changes include the use of online surveys), but our study involves participation over a two-week period with multiple “visits” and the use of electronic cigarettes. This required substantial adaption of the study methods (see below for some examples), but we were able to produce a comprehensive revision that retained the necessary components to ensure valid testing of our original research question.
We had to overcome several practical challenges, such as how to screen participants for smoking status and pregnancy. In the laboratory, we typically verify smoking status using a carbon monoxide (CO) breath monitor – equipment that cannot be used during lockdown. To overcome this, we replaced the CO monitor with a cotinine urine test, which verifies smoking status by detecting a metabolite of nicotine in urine. These are dipstick tests that participants can take themselves and we verify the outcome via a video call by asking them to show us the used dipstick.
Another challenge was how to safely deliver the e-cigarettes, e-liquids, and screening tests to participants. We are doing this via post (using pre-paid postage), with carefully constructed information packs and cleaning instructions. All test sessions that collect primary outcome data are now taking place online. This includes a cue reactivity procedure that participants are led through via pre-recorded instructions that link to our online study materials. We are also exploiting ecological momentary assessment methods (daily messaging via mobile phones) to collect real-time data across the test weeks, and all face-to-face communication has been replaced with phone and video calls. We worked closely with our faculty research ethics committee and university IT services as we developed this protocol to ensure any new ideas were feasible and ethically sound (or to identify problems early and seek alternative solutions).
Our aim was to complete a project that otherwise would not have been possible. However, the important learning point was that in developing essentially what was an “emergency response” protocol, we have unlocked other important benefits. Before the COVID-19 outbreak, our biggest challenge was recruiting participants (we require smokers who are willing to abstain from smoking for one week!). As with all university-based research, we often rely on opportunistic recruitment that means recruiting from the local area (i.e., people who can easily attend the laboratory sessions during university opening hours), and our samples often comprise a relatively high number of students. This not only means we have difficulty recruiting, but that our samples are not always representative, and our results may not generalise to the wider population. This new model of working means we have no geographical restriction (as long as the post delivers and there is Internet provision – we can collect data!), hugely improving our reach and the diversity in our participant samples.
Another benefit is that data are collected in more naturalistic settings (although this comes with a loss of control that needs to be considered or may not be appropriate for some studies). For studies that require participants to attend multiple sessions, it is also likely there will be lower attrition (i.e., fewer drop-outs) as there is less burden on participants to travel to a testing laboratory.
This has not been an easy transition (although we will certainly be well equipped to do it again if we need to). It has been time consuming, and some aspects of the study were simply not possible in the context of the fixed time constraints and funding in place, and without the laboratory facilities. The utility of this approach needs to be considered on a case by case basis. But, for our study, it was doable. We are only at the start of this process – the study will be running throughout 2020 and we look forward to the ongoing challenge and reflecting on how we can optimise this process in future.
The important take-home message is that remote research is not something we will discard after the COVID-19 restrictions are lifted. We will refine these methods and embrace the benefits they offer. Remote research will not be an emergency response option only, but instead it will be an integral part of our research toolkit.
If you are interested in finding out more, please visit our website:
http://www.bristol.ac.uk/psychology/research/brain/targ/participants/smoker-experience-ecigs/
You can also follow us on Twitter: @BristolTARG @AngelaAttwood @MaddyLDyer
Improving the way research is done: the UK Reproducibility Network
Written by Natalie Hunter, Graduate Trainee – Research Landscape at Wellcome Trust
As a graduate at Wellcome, I get the opportunity to be involved in so many exciting initiatives, including working with the people aiming to tackle some of the biggest challenges in science and research.
Attending the first annual meeting of the UK Reproducibility Network (UKRN) last Friday is a great example of this. UKRN is a grassroots, researcher-led organisation with the aim of improving scientific integrity, with a particular focus on the reproducibility of research. There’s been a lot written about the so-called ‘reproducibility crisis’ in research recently, but it essentially boils down to this: were the experiments conducted in a non-biased way, blinded where possible? Have all of the results been reported – including negative ones? Were appropriate controls used? Could the study be repeated by somebody else and the same results be found? However, it has become increasingly obvious that a number of papers, some with very influential results, have not been conducted to this standard. For example in some areas such as preclinical cancer research, studies estimate as many as 70-90% of papers have irreproducible results. This links to the wider problem of research culture we’ve identified and are working on here at Wellcome.
UKRN was founded to increase standards in research. Lead by four researchers – Marcus Munafò (Psychologist, University of Bristol), Laura Fortunato (Anthropologist, University of Oxford), Chris Chambers (Neuroscientist, University of Cardiff) and Malcolm Macleod (Neuroscientist, University of Edinburgh), the network is made up of a steering committee and two groups: Local Network Leads and Stakeholders.
The Local Network Leads are researchers, each representing a university. Together, they provide on-the-ground support within universities to help other researchers and policymakers navigate this complex area. UKRN wants local network leads to create excitement and buzz about doing high quality research. They support for example local ‘Reproducibilitea journal clubs’, where researchers collectively review research papers and discuss methodological issues.
The Stakeholders group is made up of representatives from research-related organisations, including Wellcome, UKRI, MRC, Nature, PLOS, JISC, UK Research Integrity Office, Universities UK and many more. Each organisation contributes small grants to UKRN, including Wellcome. By engaging these two key groups, UKRN aims to achieve both a bottom-up and top-down influence on UK research culture.
I attended the second half of the meeting, which was specifically for the Stakeholders. The focus of this meeting was the work plan for the year ahead. Discussion was lively, ranging from the responsibility of funders like Wellcome to those of journals such as Nature, data sharing and open access policies, the value of ‘metaresearch’ – or ‘research on research’ – and expanding discussions on these issues beyond biomedical science. The incentive structures within academia came up frequently as a key cause for concern. With publishing in a high-impact journal still seen as the key measure of success in science, despite intitives such as DORA, the concern is that pressure to publish could lead researchers to behave less than perfectly. As one attendee said, this is a “systemic issue, which needs a systemic solution”. That’s where UKRN’s strength lies. They have managed to get so many key stakeholders in a room at once to discuss these issues and commit to finding solutions that it feels like real change is on the horizon.
The potential of UKRN is exciting, and there is a sense that it is capitalising on a cultural moment in science right now; those involved feel there is a real appetite for change from a number of directions. But it’s important to remember it’s a very small organisation, with an administrator as the only paid member of staff – everybody else is involved on a purely voluntary basis. There’s only so much an organisation like that can achieve in a year. However the plans UKRN have set out for the next year are bold and ambitious: it will for example continue ongoing work (funded through the Wellcome Research on Research scheme) on linking the registered reports system with funding decisions; it will plan a large conference for next year, bringing together relevant parties for extended conversations and workshops; it will continue to grow its network and build an evidence base for improving research integrity.
So, watch this space – and the UKRN twitter account – as this network will only continue to grow and develop its influence over the coming year, with support from Wellcome and other funders.
Understanding Anorexia – Promoting Life through Prevention
An essay by Caitlin Lloyd.
Emma was an anxious child, always worrying. At thirteen, her anxiety became centered on interactions at school – she was terrified of being judged negatively by classmates. Around this time Emma began dieting, intending to lose just a small amount of weight. It turned out she could do so relatively easily, and enjoyed the sense of achievement resulting from the numbers on the scale going down. Her diet continued, becoming more and more extreme. Emma’s weight plummeted.
Eight years later, having had two inpatient hospital admissions, Emma maintains a dangerously low body weight, achieved by setting strict rules around eating. A daily calorie limit is followed, and foods containing fat and sugar avoided. Eating takes place only at certain times, and each mouthful must be chewed ten times before swallowing. Any deviation from these rules, and the day is ruined.
Emma retook two years at school, falling behind her peers, but secured a place at Durham University to study mathematics. It is difficult to concentrate on her work though, because all Emma can think about is food: what she has eaten; and what she will eat. Her focus on food makes it hard to maintain friendships, and Emma has few. Emma spends university holidays with her family, the time dominated by arguments over food.
Sometimes Emma wishes things were different. But that means eating more, which feels impossible. Deviating from the rules makes Emma unbearably anxious. No amount of support can dispel the intense fear of becoming fat, or feelings of self-disgust that accompany weight-gain.
Emma is fictional but typical of someone with anorexia nervosa, an eating disorder characterised by persistent starvation in the context of a low weight and fear of weight-gain. In the UK it is estimated that as many as one in 25 women will experience anorexia in the course of their lifetime. Men develop anorexia too; roughly one in ten people with anorexia is male.
Anorexia usually develops during adolescence, and has many adverse yet long-lasting physical and mental health consequences. Starvation compromises the function of almost all major organ systems, and feelings of despair increase the risk of suicide; anorexia has the highest death rate of any mental health disorder.
Full recovery from anorexia is a lengthy process, and unfortunately not common. Treatments exist but not one is consistently effective. Fewer than half of those diagnosed with anorexia make a full recovery, and relapse rates are high – around 30-40% of people fall back into the disorder’s grip following initial recovery. For some, weight-gain is sustained, but a strict diet and overconcern with eating and weight remains, severely impacting quality of life.
The difficulty treating anorexia makes effective prevention vital. For this we need to target the factors that cause anorexia, requiring knowledge of what those factors are. My research investigates whether anxiety disorders play a causal role in anorexia development, to help us understand whether it would be beneficial to address anxiety in young people to prevent eating disorders.
It has long been suggested that the starvation of anorexia reduces anxiety. This would make dieting helpful (in this narrow sense) to those experiencing anxiety symptoms, encouraging the dieting to continue. Anxiety disorders and anorexia often co-occur. But correlation is not causation, and determining cause-and-effect is notoriously challenging.
As an example, for anxiety to cause anorexia development, anxiety must precede anorexia. Existing findings support this, however studies have tended to ask people with anorexia to recall the time before their illness developed. Experiencing anorexia may affect memory recall; to try and explain how their anorexia developed, someone with anorexia might believe themselves to have been more anxious in childhood than they actually were. In this case the conclusion that anxiety causes anorexia may be invalid. Many sources of potential error exist in research, meaning that many findings could be inaccurate, at least to some degree.
Different research methods have different strengths and limitations, and are thus prone to different biases. This can be used to our advantage: if findings across studies of different research methods point to the same conclusion, we can be more confident the conclusion is correct. I am using a variety of research methods, each designed to minimise the potential for erroneous conclusions, to determine the role of anxiety in anorexia. If a causal role is supported across the different studies, trialing interventions designed to reduce anxiety for eating disorder prevention is encouraged. If not, the search for other factors to target for improved eating disorder prevention continues.
We are at an early stage in understanding anorexia, but we do know that many people with the illness become ill at a young age, with their whole lives ahead – like Emma. My research matters because it aims to stop people losing their lives, and quality of life, to anorexia.